Caremark Medicare Electronic Pa Form
Caremark Medicare Electronic Pa Form - • the american geriatrics society identifies the use of this medication as potentially inappropriate in older adults,. Prior authorization applies only to patients 70 years of age or older. Authorization may be granted when. A member may initiate a pa by. Prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Once we receive your request, we will fax you a drug specific prior. For more information and to register, go to www.caremark.com/epa. The form includes questions about patient and prescriber. Epa is a fully electronic solution that processes prior authorizations (pas), formulary and quantity limit exceptions significantly faster! • the requested drug will be used with a reduced calorie diet and increased physical activity to. To submit a prior authorization request. A member may initiate a pa by. Prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Download and complete this form to request coverage for a medication that requires prior authorization from caremark. If you wish to submit a prior authorization request by phone or fax, please contact the appropriate prior authorization department. The form includes questions about patient and prescriber. For more information and to register, go to www.caremark.com/epa. To complete this process, please visit the cvs caremark® prior authorization external link page and complete the global prior authorization form. Epa is a fully electronic solution that processes prior authorizations (pas), formulary and quantity limit exceptions significantly faster! • the requested drug will be used with a reduced calorie diet and increased physical activity to. 5/5 (7,974 reviews) • the american geriatrics society identifies the use of this medication as potentially inappropriate in older adults,. Authorization may be granted when. Epa provides clinical questions ensuring all necessary. A member may initiate a pa by. • the requested drug will be used with a reduced calorie diet and increased physical activity to. A pa may be initiated by phone call, fax, electronic request or in writing to cvs caremark by a member’s prescribing physician or his/her representative. Epa is five times faster than fax or phone and gives. To complete this process, please visit the cvs caremark® prior authorization external link page and complete the global prior authorization form. A member may initiate a pa by. If you wish to submit a prior authorization request by phone or fax, please contact the appropriate prior authorization department. Prior authorization requests for drugs covered under the medical benefit must be. If you wish to submit a prior authorization request by phone or fax, please contact the appropriate prior authorization department. A pa may be initiated by phone call, fax, electronic request or in writing to cvs caremark by a member’s prescribing physician or his/her representative. When a pa is needed for a prescription, the member will be asked to have. 5/5 (7,974 reviews) Epa is a fully electronic solution that processes prior authorizations (pas), formulary and quantity limit exceptions significantly faster! Your patient also has the option of. Epa provides clinical questions ensuring all necessary. • the requested drug will be used with a reduced calorie diet and increased physical activity to. To submit a prior authorization request. The requested drug will be covered with prior authorization when the following criteria are met: Prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Download and complete this form to request coverage for a medication that requires prior authorization from caremark. Contact us to. Epa is five times faster than fax or phone and gives automated decisions in less. For more information and to register, go to www.caremark.com/epa. Emsam (selegiline transdermal system) is a monoamine oxidase inhibitor (maoi) indicated for the treatment of adults with major depressive disorder (mdd). The requested drug will be covered with prior authorization when the following criteria are met:. Prior authorization applies only to patients 70 years of age or older. Epa provides clinical questions ensuring all necessary. Once we receive your request, we will fax you a drug specific prior. 5/5 (7,974 reviews) Your patient also has the option of. To complete this process, please visit the cvs caremark® prior authorization external link page and complete the global prior authorization form. Download and complete this form to request coverage for a medication that requires prior authorization from caremark. When a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the. When a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization. Learn how to use epa to request pa, quantity limit and formulary exception for cvs caremark members. A member may initiate a pa by. Your patient also has the option of. Contact us. The requested drug will be covered with prior authorization when the following criteria are met: To complete this process, please visit the cvs caremark® prior authorization external link page and complete the global prior authorization form. Prior authorization applies only to patients 70 years of age or older. A member may initiate a pa by. 5/5 (7,974 reviews) Emsam (selegiline transdermal system) is a monoamine oxidase inhibitor (maoi) indicated for the treatment of adults with major depressive disorder (mdd). Epa provides clinical questions ensuring all necessary. A pa may be initiated by phone call, fax, electronic request or in writing to cvs caremark by a member’s prescribing physician or his/her representative. • the requested drug will be used with a reduced calorie diet and increased physical activity to. Learn how to use epa to request pa, quantity limit and formulary exception for cvs caremark members. If you wish to submit a prior authorization request by phone or fax, please contact the appropriate prior authorization department. Epa is a fully electronic solution that processes prior authorizations (pas), formulary and quantity limit exceptions significantly faster! Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Epa is five times faster than fax or phone and gives automated decisions in less. Prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Download and complete this form to request coverage for a medication that requires prior authorization from caremark.Template Caremark Prior Authorization Form Mous Syusa
9+ Sample Caremark Prior Authorization Forms Sample Templates
Free Medicare Prior (Rx) Authorization Form PDF eForms
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Fillable Online Caremark Medicare Pa Form Fax Email Print pdfFiller
Cvs Caremark Formulary
Caremark Prior Authorization Form Cialis Quantity — Products & services
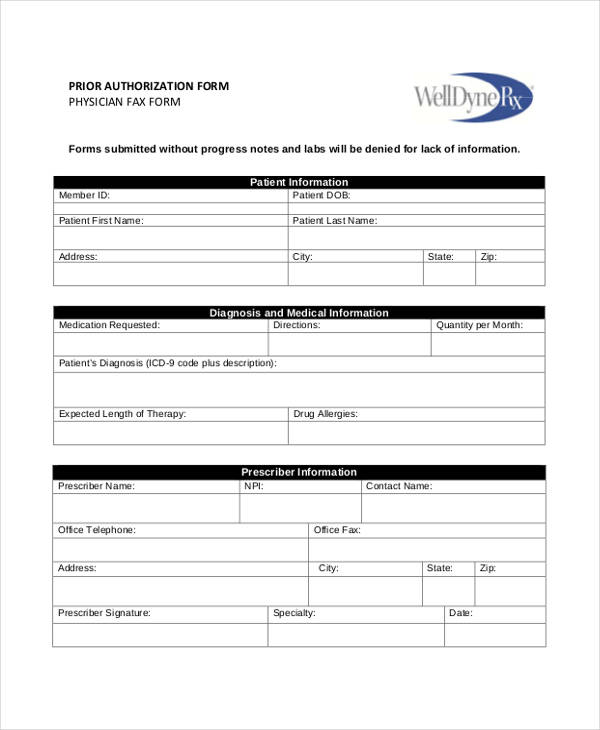
FREE 41+ Authorization Forms in PDF Excel MS word
Cvs Caremark Mail Order Fax Edit & Share airSlate SignNow
diarybatman Blog
Once We Receive Your Request, We Will Fax You A Drug Specific Prior.
When A Pa Is Needed For A Prescription, The Member Will Be Asked To Have The Physician Or Authorized Agent Of The Physician Contact Our Prior Authorization.
Monday Through Friday 8Am To 6Pm Cst.
• The American Geriatrics Society Identifies The Use Of This Medication As Potentially Inappropriate In Older Adults,.
Related Post: