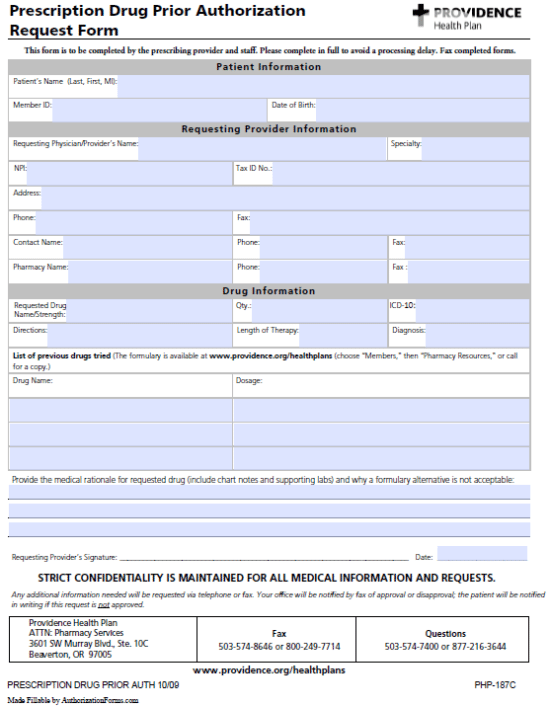
Providence Prior Auth Form
Providence Prior Auth Form - If a drug to treat your covered medical condition. Benefits are based on eligibility at the time the service is rendered and are subject to any applicable contract terms. Prior authorization request **chart notes required** please fax to: Access prior authorization guidelines, forms, and resources for providers. Non‐discrimination coordinator po box 4158 portland, or 97208‐4158 if you need help filing a grievance, and you are a. Plan forms, member authorization and privacy forms, claims and enrollment forms. Contact cvs caremark prior authorization department medicare part d. Prescription drug prior authorization r equest form this form is to be completed by the prescribing provider and staff. Access essential forms, guides, and. Click here for resources, training webinars, user guides, fax forms, and clinical guidelines for providers utilizing cohere's platform. Let us help you find the information you need. Some prescription drugs require prior authorization for medical necessity, place of therapy, length of therapy, step therapy, or number of doses. Download the evidence of coverage or annual notice of change for your providence medicare advantage plan. Benefits for services received are. Access prior authorization guidelines, forms, and resources for providers. Your doctor can submit the request online, by fax, or by phone by accessing our provider's prior authorization information. You may attach an additional page if more room is needed than provided on the request form. Request must include supporting documentation to substantiate an expedited review. Plan forms, member authorization and privacy forms, claims and enrollment forms. Use the following forms to manage authorization and access to your clients' health plan records and to request confidential communications. Your doctor can submit the request online, by fax, or by phone by accessing our provider's prior authorization information. Find out how to join the cigna healthcare network. The provider believes that waiting for a decision under the standard time frame could place the enrollee’s life, health or ability to regain maximum function in serious. This form is to be. Prescription drug prior authorization r equest form this form is to be completed by the prescribing provider and staff. Uniform prior authorization prescription request form (pdf) medical home selection if you're unsure if this applies to your providence health plan coverage, please contact customer. If you are requesting records for a deceased patient, please submit a copy of the death.. Before completing this form, please confirm the patient’s benefits and eligibility. This message is intended for the use of the person or entity to which it. This form is to be completed by the prescribing provider and staff. The provider believes that waiting for a decision under the standard time frame could place the enrollee’s life, health or ability to. Prior authorization prior authorizations made simple. If you wish to request a medicare part determination (prior. Prior authorization request **chart notes required** please fax to: Find out how to join the cigna healthcare network. Plan forms, member authorization and privacy forms, claims and enrollment forms. Benefits are based on eligibility at the time the service is rendered and are subject to any applicable contract terms. Access essential forms, guides, and. Prescription drug prior authorization r equest form this form is to be completed by the prescribing provider and staff. Click here for resources, training webinars, user guides, fax forms, and clinical guidelines for providers utilizing. Access essential forms, guides, and. The provider believes that waiting for a decision under the standard time frame could place the enrollee’s life, health or ability to regain maximum function in serious. Download the evidence of coverage or annual notice of change for your providence medicare advantage plan. Let us help you find the information you need. Prescription drug prior. Learn how providers can request precertifications for their patients. Click here for resources, training webinars, user guides, fax forms, and clinical guidelines for providers utilizing cohere's platform. Benefits for services received are. Non‐discrimination coordinator po box 4158 portland, or 97208‐4158 if you need help filing a grievance, and you are a. Before completing this form, please confirm the patient’s benefits. Prescription drug prior authorization r equest form this form is to be completed by the prescribing provider and staff. Providence health plan and providence health assurance attn: Plan forms, member authorization and privacy forms, claims and enrollment forms. Prior authorization request **chart notes required** please fax to: Let us help you find the information you need. This message is intended for the use of the person or entity to which it. Please have the following information ready when calling to request a prior authorization: Let us help you find the information you need. Learn how providers can request precertifications for their patients. Request must include supporting documentation to substantiate an expedited review. Benefits for services received are. Access prior authorization guidelines, forms, and resources for providers. Before completing this form, please confirm the patient’s benefits and eligibility. Contact cvs caremark prior authorization department medicare part d. Let us help you find the information you need. Prior authorization prior authorizations made simple. Download the evidence of coverage or annual notice of change for your providence medicare advantage plan. Prior authorization request **chart notes required** please fax to: If a drug to treat your covered medical condition. The provider believes that waiting for a decision under the standard time frame could place the enrollee’s life, health or ability to regain maximum function in serious. Your doctor can submit the request online, by fax, or by phone by accessing our provider's prior authorization information. Non‐discrimination coordinator po box 4158 portland, or 97208‐4158 if you need help filing a grievance, and you are a. Find out how to join the cigna healthcare network. You may attach an additional page if more room is needed than provided on the request form. Authorization does not guarantee benefits or payment. Request to have a printed evidence of coverage mailed to your home. Please have the following information ready when calling to request a prior authorization: Authorization does not guarantee benefits or payment. Benefits are based on eligibility at the time the service is rendered and are subject to any applicable contract terms. Use the following forms to manage authorization and access to your clients' health plan records and to request confidential communications. Plan forms, member authorization and privacy forms, claims and enrollment forms.Prolia Prior Authorization Form/ Prescription Ambetter printable pdf
MagnaCare Provider Prior Authorization Request Form
Providence Prior Authorization 20162025 Form Fill Out and Sign
Fillable Online Fillable Online Prior Authorization Request
Free Providence Health Prior Prescription (Rx) Authorization Form PDF
Prior Authorization Form ≡ Fill Out Printable PDF Forms Online
FREE 13+ Prior Authorization Forms in PDF MS Word
PDF authorization for use or disclosure of health information
Fillable Prior Authorization Form Priority Health printable pdf download
Free PriorityHealth Prior Prescription (Rx) Authorization Form PDF
Before Completing This Form, Please Confirm The Patient’s Benefits And Eligibility.
Prescription Drug Prior Authorization R Equest Form This Form Is To Be Completed By The Prescribing Provider And Staff.
Click Here For Resources, Training Webinars, User Guides, Fax Forms, And Clinical Guidelines For Providers Utilizing Cohere's Platform.
Providence Health Plan And Providence Health Assurance Attn:
Related Post: