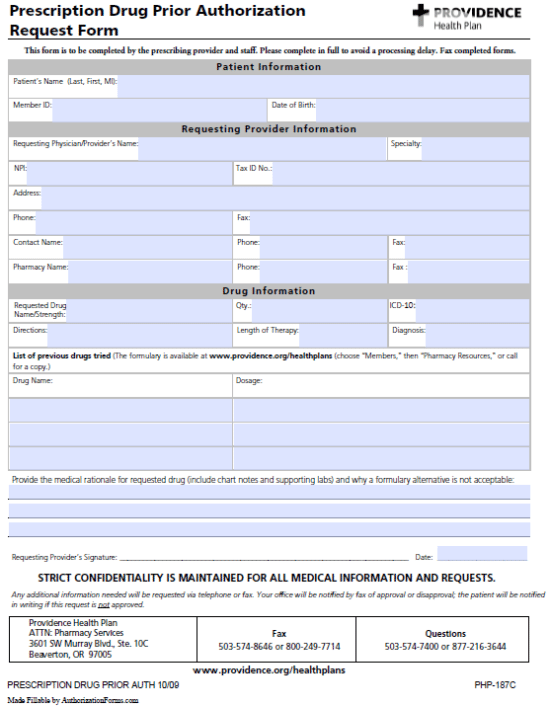
Providence Prior Authorization Form
Providence Prior Authorization Form - You may attach an additional page if more room is needed than provided on the request form. Benefits are based on eligibility at the time the service is rendered and are subject to any applicable contract terms. This form is to be completed by the prescribing provider and staff. What forms must be completed or prior authorization obtained to assure of coverage? If you wish to submit a prior authorization request by phone or fax, please contact the appropriate prior authorization department. Prior authorization request **chart notes required** please fax to: The provider believes that waiting for a decision under the standard time frame could place the enrollee’s life, health or ability to regain maximum function in serious. Documents, forms and notices for providence health plan members: Monday through friday 8am to 6pm cst. Request to have a printed evidence of coverage mailed to your home. Monday through friday 8am to 6pm cst. It includes patient, prescriber, medication, and clinical information,. For medicare advantage precertification requirements at cigna healthcare, visit our medicare advantage providers website. Request to have a printed evidence of coverage mailed to your home. The form also includes non. Fill in the patient, provider, drug and medical rationale information and fax the. The provider believes that waiting for a decision under the standard time frame could place the enrollee’s life, health or ability to regain maximum function in serious. You need to provide patient, provider, pharmacy and drug information, as well as. Plan forms, member authorization and privacy forms, claims and enrollment forms. Download and print the form to request prior authorization for certain prescription drugs covered by providence health plan or providence health assurance. Download and print the form to request prior authorization for certain prescription drugs covered by providence health plan or providence health assurance. If you wish to submit a prior authorization request by phone or fax, please contact the appropriate prior authorization department. Let us help you find the information you need. Documents, forms and notices for providence health plan members:. For medicare advantage precertification requirements at cigna healthcare, visit our medicare advantage providers website. Fax or call the numbers provided and include the required information and documentation. Documents, forms and notices for providence health plan members: The provider believes that waiting for a decision under the standard time frame could place the enrollee’s life, health or ability to regain maximum. You can also download it, export it or print it out. You need to provide patient, provider, pharmacy and drug information, as well as. Authorization does not guarantee benefits or payment. What forms must be completed or prior authorization obtained to assure of coverage? Download and print the form to request prior authorization for certain prescription drugs covered by providence. Let us help you find the information you need. Please complete in full to avoid a processing delay. Download and print the form to request prior authorization for prescription drugs from providence health plan. Documents, forms and notices for providence health plan members: Learn how to select a medical home provider,. Prior authorizations shouldn’t slow down patient care. You, your representative or your doctor can ask us for a coverage decision by calling, faxing or mailing your request to us. Download and fill out this form to request prior authorization for certain services or items. Up to 40% cash back send providence health plan prior authorization form via email, link, or. This form is to be completed by the prescribing provider and staff. The form also includes non. Benefits are based on eligibility at the time the service is rendered and are subject to any applicable contract terms. If you are requesting records for a deceased patient, please submit a copy of the death. Monday through friday 8am to 6pm cst. Request to have a printed evidence of coverage mailed to your home. Learn how to select a medical home provider,. You, your representative or your doctor can ask us for a coverage decision by calling, faxing or mailing your request to us. Benefits are based on eligibility at the time the service is rendered and are subject to any applicable. You can also download it, export it or print it out. Find the forms and documents you need for your providence health plan membership, including prior authorization prescription request form. Use the following forms to manage authorization and access to your clients' health plan records and to request confidential communications. If you wish to submit a prior authorization request by. Request to have a printed evidence of coverage mailed to your home. Download and fill out this form to request prior authorization for certain services or items. Authorization does not guarantee benefits or payment. You, your representative or your doctor can ask us for a coverage decision by calling, faxing or mailing your request to us. Please complete in full. You may attach an additional page if more room is needed than provided on the request form. If you wish to submit a prior authorization request by phone or fax, please contact the appropriate prior authorization department. Learn how to select a medical home provider,. You, your representative or your doctor can ask us for a coverage decision by calling,. Find out what services require prior authorization, how to request it, and what to do. Download and fill out this form to request prior authorization for certain services or items covered by your providence health plan. What forms must be completed or prior authorization obtained to assure of coverage? Find the forms and documents you need for your providence health plan membership, including prior authorization prescription request form. The provider believes that waiting for a decision under the standard time frame could place the enrollee’s life, health or ability to regain maximum function in serious. Monday through friday 8am to 6pm cst. Use the following forms to manage authorization and access to your clients' health plan records and to request confidential communications. Prescription drug prior authorization r equest form this form is to be completed by the prescribing provider and staff. Learn how to get approval from providence health plan for some services or treatments before they occur. Prior authorizations shouldn’t slow down patient care. The form also includes non. Please complete in full to avoid a processing delay. For medicare advantage precertification requirements at cigna healthcare, visit our medicare advantage providers website. It includes patient, prescriber, medication, and clinical information,. Download and fill out this form to request prior authorization for certain services or items. Let us help you find the information you need.Fillable Online Provider update Prior Authorization Request Form Fax
Providence Prior Authorization 20162025 Form Fill Out and Sign
Fillable Online Fillable Online Prior Authorization Request
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Prolia Prior Authorization Form/ Prescription Ambetter printable pdf
Fillable Online Prior Authorization Requirements Anthem Providers Fax
Free Providence Health Prior Prescription (Rx) Authorization Form PDF
FREE 10+ Sample Authorization Request Forms in MS Word PDF
Fillable Standard Prior Authorization Request Form United Healthcare
Fillable Online Providence Health Plan Prior Authorization Form 2016
Documents, Forms And Notices For Providence Health Plan Members:
You Need To Provide Patient, Provider, Pharmacy And Drug Information, As Well As.
You Can Also Access Our Medicare Advantage Prior.
This Form Is To Be Completed By The Prescribing Provider And Staff.
Related Post: